Investigation of the causes of recurrent miscarriage

Sperm chromatin fragmentation tests (TUNEL and SCSA)

Non-invasive prenatal testing (NIPT)
History of NIPT In the past, it was not possible to examine a fetus during pregnancy and prevent the birth of babies with chromosomal disorders.
In today’s era of advanced medical and laboratory techniques, healthcare professionals including geneticists, obstetricians, and perinatologists recommend ultrasound and blood screening tests during the first and second trimesters of pregnancy for fetal monitoring. Despite these advancements, these screenings cannot detect all fetal abnormalities with 100% accuracy.
If the results of these screening tests are positive (approximately 5-10% of the tested population), genetic testing of the fetus using amniotic fluid is considered. Amniotic fluid surrounds the fetus during pregnancy. When these tests indicate a high risk, genetic testing of the fetus by collecting fetal cells from a sample of this amniotic fluid is the suggested approach, known as amniocentesis.
Amniocentesis is performed by a perinatologist. After isolating the fetal cells present in the fluid and extracting their DNA or culturing the cells, the fetus’s chromosomal abnormalities are examined through molecular and microscopic analysis.
This procedure is not without risks. The process of collecting amniotic fluid can pose dangers to both the mother and fetus, including miscarriage (approximately 0.5-1% of cases), bleeding, rupture of the membranes, and infection of the membranes surrounding the fetus.
Advantages of the NIPT test compared to other methods
Fortunately, today we have a very low-risk method to access fetal DNA, and the cell-free DNA test or NIPT has made this possible. One of the drawbacks of first and second-trimester screening tests is the high rate of false negatives. This means that many women who receive low-risk results may still give birth to babies with Down syndrome or other chromosomal abnormalities.
Non-invasive prenatal testing (NIPT) is a method that, with a simple blood draw from a pregnant woman, can be used from the 10th week of pregnancy onwards to determine the risk of a fetus being born with specific chromosomal abnormalities, such as trisomy 21, trisomy 18, trisomy 13, and also to determine the sex of the fetus. This test examines small pieces of fetal DNA that circulate in a pregnant woman’s blood. Unlike most DNA found in the nucleus of a cell, these fragments are not found inside cells but are floating and free, which is why they are called cell-free fetal DNA (cffDNA).
These fragments are usually less than 200 DNA building blocks (base pairs) long and are formed when cells die and their contents, including DNA, are released into the bloodstream. cffDNA is shed into the maternal bloodstream from the cells of the fetal placenta and is usually identical to the fetal DNA. Therefore, analyzing cffDNA fragments provides an opportunity to detect some chromosomal abnormalities early without harming the fetus.
Another advantage of NIPT is that it has a much lower false positive rate compared to combined first and second-trimester screening. This means that fewer patients will need chorionic villus sampling or amniocentesis to confirm a high-risk result, and this puts fewer mothers at risk of miscarriage, as both chorionic villus sampling and amniocentesis are associated with a risk of secondary miscarriage.
What is the best time to do the NIPT test?
As mentioned, during pregnancy, small amounts of cffDNA circulate in the mother’s bloodstream. This amount varies throughout pregnancy but peaks in the late first and early second trimesters. Therefore, the best time to perform the NIPT test is after the 10th to 12th week of pregnancy and after an ultrasound to measure the thickness of the fluid behind the neck of the fetus (NT ultrasound).
However, NIPT can be performed at any stage of pregnancy after the 10th week, especially if an anomaly ultrasound at 18-20 weeks indicates a high risk of trisomy 21, trisomy 18, or trisomy 13 and there are concerns.
Who should have the NIPT or cell-free DNA test?
- Pregnant women whose screening test results are positive (high risk) or in the risk range (moderate risk).
- Pregnant women who are advanced maternal age.
- Pregnant women who have a child with Down syndrome or other chromosomal disorders.
What does it mean if your NIPT test result is high risk?
Since NIPT is a screening test rather than a diagnostic test, if it shows a high risk or aneuploidy for chromosomes 21, 13, 18, X, or Y, it does not mean that your fetus definitely has one of these defects. There is a chance of a false positive result for each of these tested chromosomes.
Therefore, consult with your doctor about an ultrasound and a diagnostic test such as chorionic villus sampling or amniocentesis to assess possible chromosomal abnormalities that may help in diagnosis. After a definitive and final diagnosis, you can make a decision about your pregnancy.
What does it mean if your NIPT test result is low risk?
If NIPT shows a low-risk or no aneuploidy result, it means that your fetus is unlikely to have a chromosomal problem related to chromosomes 21, 13, 18, X, or Y. However, since NIPT does not detect all (100%) chromosomal abnormalities, even if the NIPT results are reassuring, your doctor may suggest additional tests such as amniocentesis if your fetal ultrasound shows structural abnormalities or other concerning features.
Therefore, even if the NIPT results are reassuring, if your fetal ultrasound shows structural abnormalities or other concerning features, your doctor may suggest additional tests such as amniocentesis.
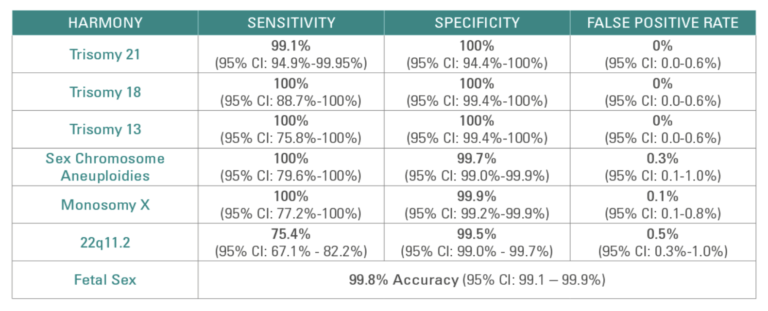
The table below shows the sensitivity and specificity of testing for disorders of each of these chromosomes in the NIPT test. It is worth noting that recently, testing for microdeletions including 11.2q22 (DiGeorge syndrome), Angelman syndrome, Prader-Willi syndrome, and Cri du Chat syndrome has also become available with some forms of NIPT.
Limitations of the NIPT test
- This test cannot be performed in triplet or higher-order pregnancies.
- The sensitivity and accuracy of this test are lower in twin pregnancies.
- This test cannot be reported for pregnancies less than 10 weeks.
- Despite its high accuracy, this test cannot detect all chromosomal abnormalities, including mosaicism.
- This test cannot detect abnormalities in the number of sex chromosomes, such as Turner syndrome and Klinefelter syndrome.
- This test is a screening tool, and a positive result (high risk) must be confirmed by other diagnostic methods such as CVS and amniocentesis.
- A negative test result (low risk) in pregnant women cannot guarantee a completely healthy pregnancy.
- In a small number of pregnant women, the amount of free fetal DNA in the blood is very low, and in some cases, even with repeated testing and blood draws, satisfactory results cannot be obtained.
- In pregnant women weighing over 100 kg or with a high BMI, the likelihood of obtaining inconclusive results is much higher.